Safer surgeries with microbots
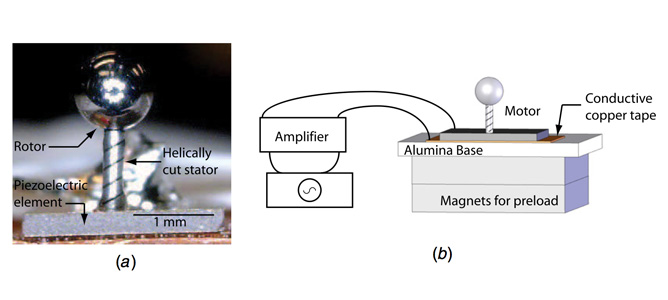
a) Photo of the micro-motor prototype showing the helically cut stainless steel ball as a rotor and the PZT element. b) Magnets were used to increase the friction coupling preload
March 2012
The future is here - microrobots are making minimally invasive vascular surgery safer and more efficient.
Researchers at MCN have developed a 240μm-diameter ultrasonic micromotor capable of navigating through arteries deep inside the human body. The technology, developed by Professor James Friend of RMIT University, is designed to assist surgeons whilst performing minimally invasive vascular surgery (MIVS).
The ultrasonic micromotor comprises a 50μm-diameter stainless steel ball rotor mounted on a laser machined precision tube, prepared at the ANFF OptoFab node. The stainless steel ball is held in place using a magnetic payload generated from a permanent magnet, allowing it to make contact with the inner diameter of the tube. According to Professor Friend, the micro-sized motor generates rotational motion from a combination of orthogonal and longitudinal vibration modes. The drive’s input signals are provided via two 50μm diameter wires. The micromotor assembly is designed to be affixed to standard catheter tips, providing smooth navigation through vascular pathways.
This technology has several advantages over existing MIVS techniques that traditionally have a failure rate of up to 40%. The first major advantage is that the catheter guide wire is actively navigated using a motor, rather than being forcibly pushed through arterial passages. This is likely to result in a reduction in injury to vascular membranes. Further, complex cerebral events (such as an aneurism) have a time-sensitive treatment window. This technology allows medical specialists to locate and treat the cerebral event up to 20% faster than conventional MIVS procedures.
In addition, Professor Friend notes that modelling shows that up to 85% of 350μm cerebral arteries can be accessed easily with this novel micromotor because its tip size is less than 250μm. Combined with an additional 4 cm of reach, this technology provides opportunities for treatment well outside the scope previously available.
A simulated video can be viewed here.